The Case for Mask Mandates
A review of Canada's current post-mandate status, evidence supporting temporary and targeted mask mandates, and critical success factors.
There are five sections, click a section to skip to it:
1. Canada’s current situation
The Canadian public has mostly moved on from masking in public spaces and schools since mandates were dropped in the Winter and Spring of 2022 and individuals were advised to “wear a mask if it’s right for them”. Masking adherence has dropped from 70% to under 10% since the mandates were removed.
I believe the intent was to recognize that many had been infected in the December - February Omicron mass infection wave and together with vaccinations had boosted immunity. There was also the general assessment that Omicron was milder and few under the age of 60 would face severe outcomes while those over 60 could protect themselves. As the Premier of Ontario said in February, “I’m done with covid!”.
The messaging from provincial governments and public health was clear: the worst of the storm had passed. The public was asked to make their own personal risk assessments. Unfortunately, that was difficult given the lack of public health guidance and data on how to actually do that.
In Canada, the dropping of general PCR testing and the lack of reporting on deaths and long covid meant that many Canadians were unaware of their risk, even misled by charts from their public health leaders who continued to present massively underreported Omicron case trends — the pre-Omicron case trend was based on normal PCR testing rates while the Omicron period was based on minimal testing.
How 2022 is playing out
The expectation of a more normal 2022 after masks and other measures were removed was at best premature.
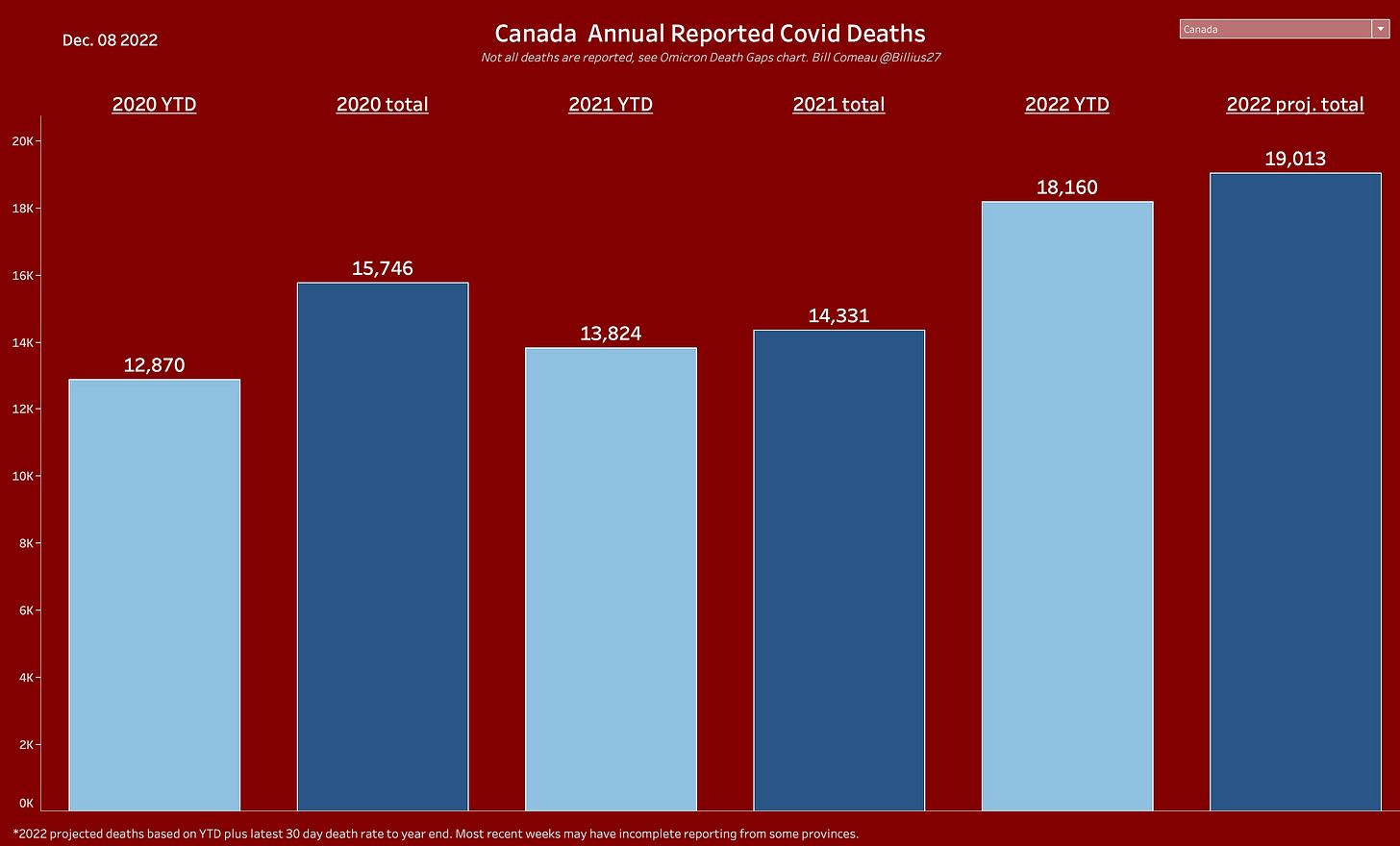
Covid deaths are underreported according to the work of Dr. Tara Moriarty but I will use the official accounting. Deaths are running far ahead of 2020 and 2021 and are projected to reach 19,013 compared to 14,331 in 2021.
Hospitalizations are far ahead of previous years as well. Even if we, for sake of argument, completely ignored hospitalizations where covid was detected in patients admitted for other conditions, the current level continues to run above the 2020-2021 pre-Omicron average of 1,961.
Infections with Omicron are much higher than previous years. And therein lies the problem. The combination of vaccinations, boosters, prior infections, treatments, and variants that are less severe per infection should in theory lower the level of severe outcomes. But they don’t.
While we are protected to some degree by all the positive factors I just listed, there are three missing factors:
Omicron is more transmissible - it takes fewer minutes of exposure to become infected and the incubation time to become infectious is shorter
Omicron is better at evading our immune system - vaccines are less able to protect against infection than Delta, and vaccine and infection-boosted immunity also wanes over time. After 3 months, a covid booster provides under 60% protection against symptomatic infection (see chart below), the same as a flu shot. (This is one reason masks are important tools to complement vaccines and help reduce spread.)
The relaxation of masking and other precautions has helped Omicron infection rates stay high.
These three factors have combined to push Omicron infections to constantly high levels. The current estimate is that over 70% of Canadians have been infected by Omicron up to October 15th based on blood sample seropositivity testing.
This fairly constant and elevated level of infections are currently estimated at 78,894-195,296 per day. The net result is the severe outcomes we see in the above charts, they are the result of a simple calculation.
Total severe outcomes = average severity per infection times number of infections.
Herd Immunity
When mask mandates were dropped, public health officials explained that many now had good immunity protection after being vaccinated and infected. But Omicron variants have proven to be evasive and many Canadians have been reinfected, especially as their immunity protection wanes over time. This England chart shows how reinfections increasingly contribute to total infections in a country that has been highly vaccinated and highly infected by Omicron:
Long covid - the shadow epidemic
Besides 2022 being a record year for severe outcomes, 10.5% of Canadians are reporting long covid symptoms three or more months after an Omicron infection. The UK is estimating 2.2 million people have long covid. The US Brookings Institute has estimated 2-4 million out of work in the US due to long covid. A major US study published in Nature last month also identified long covid risk increased with the number of cumulative reinfections.
Compared to no reinfection, reinfection contributed additional risks of death (hazard ratio (HR) = 2.17, 95% confidence intervals (CI) 1.93–2.45), hospitalization (HR = 3.32, 95% CI 3.13–3.51) and sequelae including pulmonary, cardiovascular, hematological, diabetes, gastrointestinal, kidney, mental health, musculoskeletal and neurological disorders. The risks were evident regardless of vaccination status.
There are now a host of studies documenting long covid (or PASC) impacts on various organ systems.
There is much still to learn about long covid in Canada, especially given the lack of tracking and data reporting but at a minimum we are likely looking at wide-ranging population, health system, and economic impacts as infections and reinfections mount. The Ontario Science Table produced a brief, here is an excerpt:
The post COVID-19 condition poses substantial health risks across a diverse range of outcomes that may result in a considerable burden for Ontarians, the economy, and the healthcare system.
Like deaths, there is evidence that Omicron long covid outcomes are milder per infection, especially after vaccination, but again, the sheer volume of infections leads to concerns about the scale of the problem in Canada. This risk has been compounded by the removal of masks and other precautions like isolation requirements, since preventing a (re)infection prevents long covid risks from that (re)infection.
The rise of respiratory viruses
The first Fall season without school mask requirements in many provinces since the pandemic began is seeing extraordinary and unprecedented surges in pediatric hospitalizations. Here are the current influenza-associated pediatric hospitalizations in blue compared to previous years.
Here is the current status of Ontario’s pediatric ICUs as hospitals attempt to expand capacity. Essentially, hospitals are in crisis mode.
An Ottawa children’s hospital has made an unprecedented call on the Red Cross for assistance. Despite a plea from the chief of the staff of the hospital, an Ottawa school board chose to not pass a mask requirement for their schools, in part due to the lack of updated guidance and action at the provincial level.
Severe cases of RSV and influenza are surging above historical norms. At the same time we know mask use is at a pandemic low. It is difficult to report on Omicron infections in schools because they are no longer tested or tracked and isolation requirements are relaxed. A BC seropositivity study found the highest infection rates among school-aged children. Mask requirements were removed part way through this school year.


Impact of dropping mask mandates
Allow me to condense all of this into a few back-of-the-envelope approximate estimates using the Canadian post-mandate data plus working assumptions that continued mask mandates would have resulted in a 20%* reduction in infections and deaths and a related reduction** in long covid rates.
(*The Institute of Health Metrics and Evaluation estimates 80% mask use can reduce transmission by 30%; ** I am conservatively assuming only half of the Stats Canada 10.5% long covid symptom report rate since we have no control group to adjust for symptoms that may have occurred without covid.)
If mask mandates had not been dropped, right now we could be looking at roughly 4.4 million fewer infected by Omicron, 2,300 fewer Omicron deaths, 230,000 fewer long covid cases, and of course fewer child respiratory illnesses that are currently overwhelming children’s hospitals.
I have yet to find an expert who suggests the upcoming winter season is not going to be very difficult for Omicron, other respiratory illnesses, and hospitals. Continuing a mask optional policy that has led to 90% or more of the Canadian population without masks while facing greater rates of airborne respiratory viruses during the winter is highly questionable at least.
Let’s take a look at the evidence.
2. Mask mandate evidence
Introduction
For scientific evidence supporting airborne transmission, two-way risk, masks themselves and advice on mask selection and use, I have written an article, “The science behind masks and their use”.
Before I review mask mandate research, I want to re-emphasize a few things that may get lost in mask discussions that assume individual choice allows people who choose to mask to protect themselves. The argument that taking off a mask indoors does not affect the risk to others is not founded in science. CIDRAP and others have studied this. While the minutes are approximate and pre-Omicron when time to infection was longer, the relative risk is based on research. This is why teamwork reduces transmission risk more than solo efforts.
Another misconception is that people know when they are infected so can help protect others by just wearing a mask when they know they are infectious. This is also untrue. Approximately half of Omicron infections are believed to be asymptomatic.
Misinformation
First a word on viral social media. One source of confusion and misinformation is the sharing of case trend charts that show cases rising when people were masking. This is a basic statistical fallacy and a reason why we need careful studies: you can’t assess a public health measure like mask mandates without some estimate or control group on what would have happened if mask mandates had been dropped. Whatever rise was seen in a case trend, the science on masking and mandates would expect it to be even steeper and higher if mandates were not in place. Here is an -illustration only- of what I mean: all curves rise with or without masking but masking is expected to slow the rise.

There have been various disinformation campaigns to support the dropping of masks and other precautions, including “herd immunity”, “vaccines are unsafe”, and more recently, “immunity debt”. The latter has been specifically used to dissuade parents from masking their children as children’s hospitals are under duress. This thread helps debunk dangerous “immunity debt” narratives.
One study that gained a lot of attention was a Danish RCT (#4 in Appendix) that viral campaigns pointed to as proof that masks and mandates do not work. However, it was not designed to answer either question and the authors made that clear. It had major design limitations as far as assessing masks or mask mandates. In fact it was not a mask mandate study at all. More feedback here and here.
It did not test during times of higher infection rates, had no means to detect changes in viral spread beyond the individual wearer, only looked at handing out and recommending masks, did not track compliance, and had insufficient sample to detect a practical mask effect. Public Health Ontario experts had this to say:
This study does not provide evidence that public mask wearing is ineffective for controlling COVID-19 through source control. The summation of the current body of evidence on mask use strongly supports public mask mandates as effective in controlling community transmission of COVID-19.
Research Review
I have compiled a list in the Appendix of 33 studies, reviews, and reports from well-respected scientific journals and official sources like the CDC and Public Health Ontario with links and key excerpts. For the studies, a priority was placed on peer-reviewed and published articles in major journals. It’s not complete, there are likely more, and most studies were pre-Omicron when case testing and reporting allowed greater analysis, but they paint a picture: mask mandates are a useful tool to reduce transmission and where analyzed, also show reduced hospitalizations and deaths.
Let’s look at some of that evidence.
Bangladesh
One of the best known is a large scale randomized controlled trial (RCT) conducted by Stanford and Yale universities, (#11, appendix).
The researchers enrolled nearly 350,000 people from 600 villages in rural Bangladesh. Those living in villages randomly assigned to a series of interventions promoting the use of surgical masks were about 11% less likely than those living in control villages to develop COVID-19, which is caused by infection with the SARS-CoV-2 virus, during the eight-week study period. The protective effect increased to nearly 35% for people over 60 years old. - Stanford Medicine News
While an 11% reduction with surgical masks may seem modest, keep in mind that this was achieved without mandates and with mask wearing only increasing from 13.3% in control villages to 42.3% in treatment villages. Very importantly, those over 60 saw a 35% reduction.
Our results should not be taken to imply that mask-wearing can prevent only 10% of COVID-19 cases, let alone 10% of COVID-19 mortality. Our intervention induced 29 more people out of every 100 to wear masks, with 42% of people wearing masks in total. The total impact with near-universal masking—perhaps achievable with alternative strategies or stricter enforcement—may be several times larger than our 10% estimate.
Country Comparisons
A world-wide natural experiment occurred early in the pandemic that allowed a comparison between 27 countries with and 17 countries without face mask mandates in nearly 1 billion (911,446,220 total) people. The study published in April 2022 applied a longitudinal mixed effect modelling approach to help remove confounding factors. Significantly higher mortality rates were found in countries without face mask mandates.
Average COVID-19 mortality per million was 288.54 in countries without face mask policies and 48.40 in countries with face mask policies… A total of 60 days into the pandemic, countries without face mask mandates had an average daily increase of 0.0533 deaths per million, compared with the average daily increase of 0.0360 deaths per million for countries with face mask mandates.
States, Counties, and Cities
There is considerable evidence, particularly from the US, that mask mandates were associated with the reduction of Rt, cases, and hospitalizations in the first two years of the pandemic.
A US study used difference-in-difference and event modelling to look at the association of county-level hospitalizations and state mask mandates early in the pandemic. State-issued mask mandates were associated with a reduction in COVID-19 hospitalizations. Event study results suggest that this association increased the longer mask mandates were in effect.
Rt decreased in five western US states after the introduction of mask mandates. In Oklahoma: “Compared to rates in communities without mask mandates, transmission rates of SARS-CoV-2 slowed notably in those communities that adopted a mask mandate.” The CDC reported on reduced case rates based on segmented regression in Kansas counties that had mask mandates. Lifting the mask mandate in Iowa was associated with an increase in new COVID-19 cases. The authors conclude: “Caution should be applied when making this type of policy decision before having achieved a more stable control of the pandemic.”
A larger observational US-wide study found that in 412 US counties between March - October 2020, on average the daily case incidence per 100,000 people in masked counties compared with unmasked counties declined by 35 percent at six weeks.
The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in Melbourne Australia. In Hong Kong: “We conclude that universal mask-wearing can reduce transmission, but transmission can continue to occur in settings where face masks are not usually worn.”
Schools and Universities
An important and compelling study given its relevance to the dropping of school masking requirements in Canada was published last month in the New England Journal of Medicine. It analyzed the impact of lifting requirements in Massachusetts in February 2022 during Omicron. It was only possible because two school districts (Boston and Chelsea) did not follow the state’s rescinding of universal masking requirements in schools.
A comparison between schools with and without masking requirements shows that schools that dropped the requirements had higher case rates over the rest of the school year and in fact one-third of their cases were associated with the decision to drop masking requirements. This social media thread also summarizes why the impact of dropping masks may have actually been underestimated in the Boston study. The study summarizes its key findings:
“Among school districts in the greater Boston area, the lifting of masking requirements was associated with an additional 44.9 Covid-19 cases per 1000 students and staff during the 15 weeks after the statewide masking policy was rescinded. This estimate corresponded to an additional 11,901 Covid-19 cases (95% CI, 8651 to 15,151), which accounted for 33.4% of the cases (95% CI, 24.3 to 42.5) in school districts that lifted masking requirements and for 29.4% of the cases (95% CI, 21.4 to 37.5) in all school districts during that period.”
The timing of the Massachusetts mandate-dropping decision was similar to what occurred across Canada. Alberta dropped mandates in February, Ontario in March. Neither produced evidence in support of their decisions, although documents released after a court order showed that Alberta school boards with mask mandates at the start of the school year had an average of 7.3 outbreaks and those without had an average of 23.4 outbreaks.
The Boston study was the most recent but there is much more school evidence.
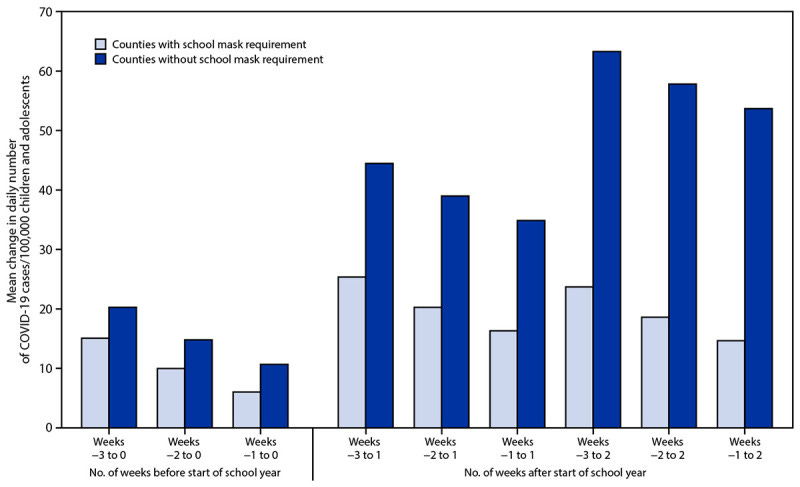
This report by the CDC highlights the substantial reduction in pediatric cases at the start of the 2021 school year in US counties with school mask requirements.
There are more school mandate studies in the Appendix: Arkansas (CDC MMWR), Texas #1, Texas #2 , and Spain.
The Arkansas study compared school districts with full or partial mask policies to those without and found higher covid incidence rates in those without mask policies. The Texas #1 study found lower covid test positivity among students in schools where masks were required. The Texas #2 study found lower covid incidence where masks were required. The Spanish study compared 5 year olds in preschools without mask mandates to 6 year olds in primary schools with mask mandates. They detected no mask benefit when comparing the two groups.
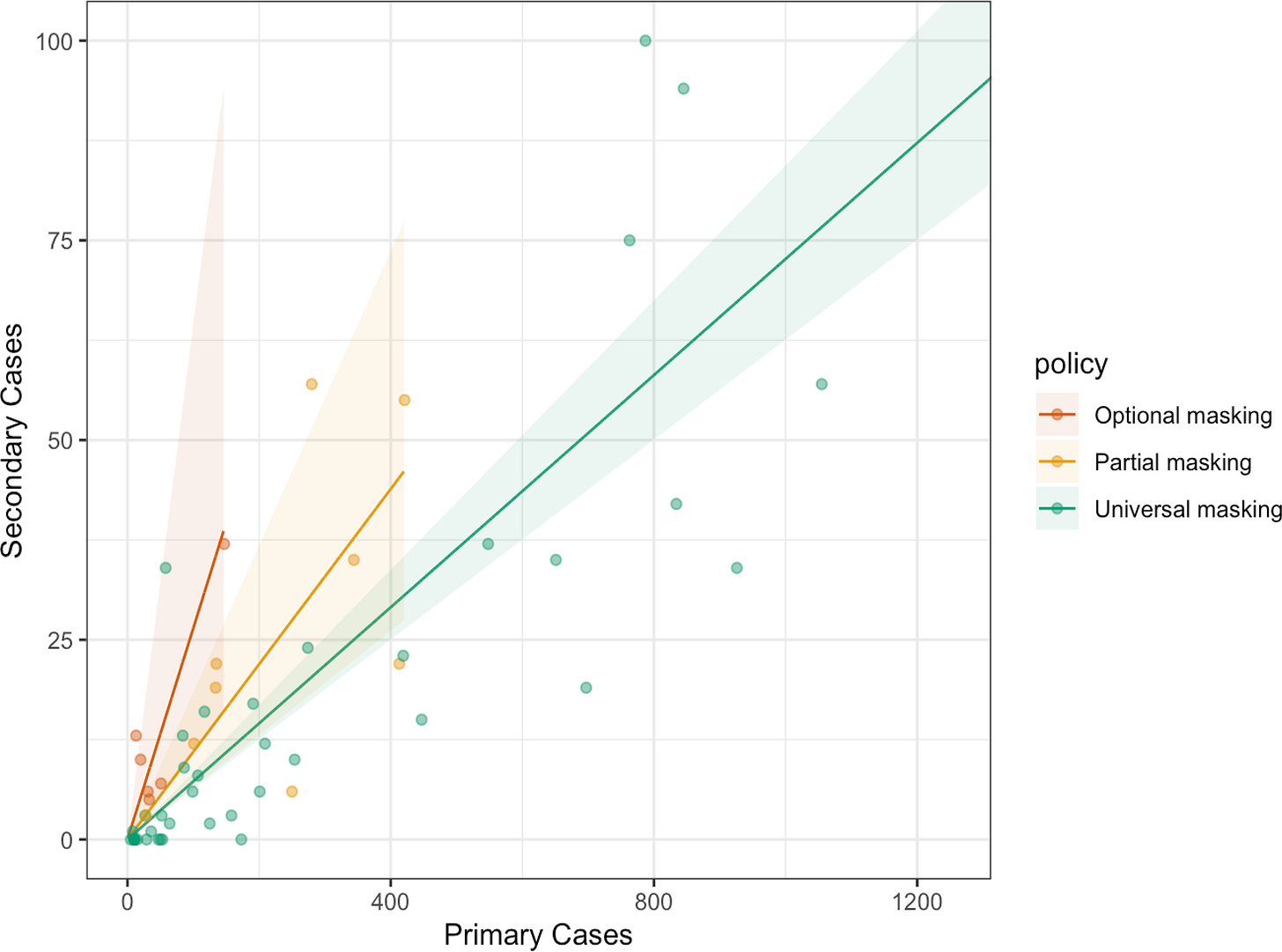
The 70,000 member American Academy of Pediatrics highlighted a paper on secondary infections published in Pediatrics. In a July-December 2021 national, prospective, observational, open cohort study of 61 K-12 school districts, involving over one million students and staff, the authors found “for every 100 community-acquired cases, universally masked districts had 7.3 predicted secondary infections, whereas optionally masked districts had 26.4.”
There are also physical science studies that highlight the benefits of school mask wearing in combination with other measures like ventilation and filtration:
“The use of moderate to high EFE masks reduces infection probability, >5× in some cases. Reductions provided by ventilation and masks are synergistic and multiplicative.”
“In the absence of interventions, the cumulative dose absorbed was 1.5 times higher in winter than in spring/summer”, “Surgical face masks were very effective independently of the season (8-fold decrease). Combined interventions (i.e., natural ventilation, masks, and HEPA filtration) were the most effective (≥25-fold decrease)”
An exhaustive Fall 2021 cohort study (during Delta) at Boston University utilized 600,000 PCR surveillance tests and looked at the likelihood of in-class transmission based on students in the same class and utilizing genomic testing. Of more than 140 000 in-person class events and a total student population of 33,000, only 9 instances of potential in-class transmission were identified, accounting for 0.0045% of all classroom meetings. The authors conclude: “These results suggest that in-class transmission of SAR-CoV-2 in an urban university with masking and vaccine protocols in-place was negligible.”
General relationship between higher population mask wearing and reductions in transmission
Stepping back from individual studies of mandate effectiveness, it is important to understand the goal of a mandate: the goal is to reduce community transmission risk by increasing the use of an evidence-based protection — mask wearing.
An important study out of Princeton and published in the Proceedings of the National Academy of Science in May 2022 looked at 92 regions across six continents and a survey of 20 million people on mask wearing. A Bayesian modelling approach adjusted for other interventions like bans on large gatherings and estimated that average mask wearing levels themselves reduced the population’s virus reproduction number by 19%.
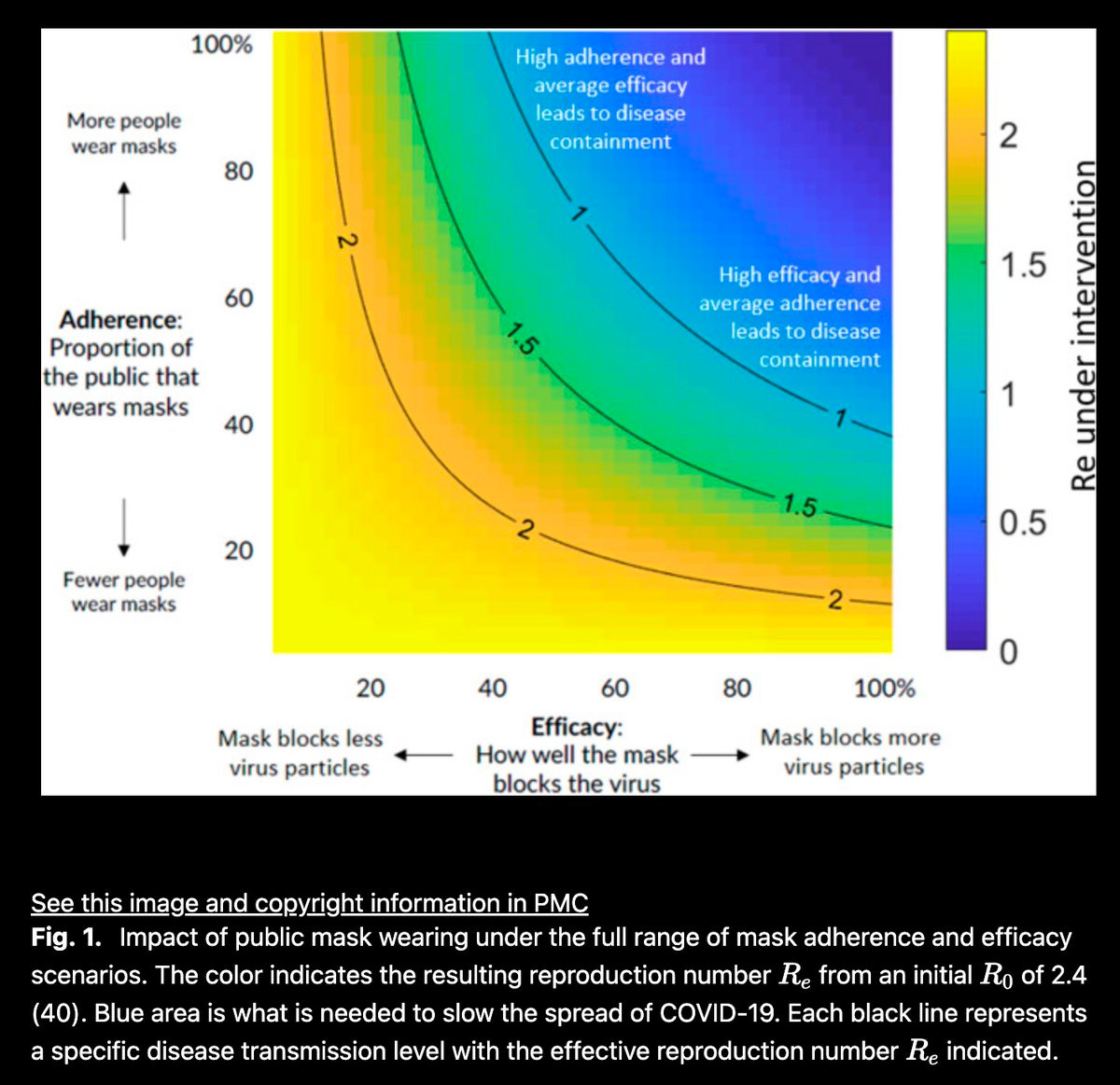
Other work shows how the combination of more people wearing masks (vertical scale) and greater mask effectiveness can combine to reduce the ability of the virus to spread.
Respiratory Viruses and Masking
This highly cited systematic review and meta-analysis published in 2020 shows that masking is protective against respiratory viruses for both HCW and non HCW. Another study examined the use of within-household masking and found “adherence to mask use significantly reduced the risk for ILI-associated infection, but <50% of participants wore masks most of the time. We concluded that household use of face masks is associated with low adherence and is ineffective for controlling seasonal respiratory disease”.
Potential side effects of child school masking
In an ideal world, children would not be masking. If there was no risk, there would be no reason to mask. Unfortunately there are times when masking is required to prevent further harm to children, including fewer days out of school sick in isolation or in hospital. But we also need to consider any potential side effects from masking in making that decision.
A review of mask wearing in children in August 2022 by Public Health Ontario concluded:
“Studies have shown that schools with masking policies have been associated with lower incidence of severe acute respiratory coronavirus 2 (SARS-CoV-2) infection compared to schools without mask mandates for children.
“Studies evaluating child adherence to masking policies have shown similar results in school … with increased adherence as age increased.”
“no objective evidence for reduced respiratory function in children who wore masks, with commonly reported complaints being subjective…. no evidence of negative cognitive impacts and … mixed results for studies on the psychological, communicative and dermatologic impacts of child mask-wearing.”
The American Academy of Pediatrics supports masking for children 2 and older and answers common questions parents have here: HealthyChildren.org. From a National Geographic article entitled “Do Masks Harm Kids? Here’s what the science says.”
“But we do have this human experiment that’s been going on with kids wearing masks at school, and we know that we haven’t seen those fears of health risks realized,” says Theresa Guilbert, a pediatric pulmonologist who is a member of the American Academy of Pediatrics
The same National Geographic article goes on to interview more experts and review areas like social and language development. The current evidence is mixed, with experts still debating the limited research. This media article by Global News interviewed experts on child masking, their consensus was that masks are not harming kids.
An expert on cognitive and social development was interviewed by the NY Times:
”Even parents who support mask mandates often worry about how a school year without smiles and frowns might negatively affect their children. These concerns are understandable but unwarranted. Although scientists don’t have much data yet on how wearing masks during a pandemic affects children’s development, there is plenty of reason to believe that it won’t cause any harm.” Dr. J. Danovitch, research psychologist who studies the cognitive and social development of children.”
A small German study found no difference when cognitive tests were conducted.
“Overall, there were no significant differences in cognitive performance between both groups, masks vs. no masks. Wearing face masks has no significant influence on attention and executive functions of pupils and can still be recommended during school lessons.”
Mask Mandates, Public Attitudes, and Behaviour
A US study observed the masking behaviour of 109,999 individuals in 126 US cities, 48% wore masks correctly. Having a local mask mandate increased the odds of wearing a mask by nearly 3-fold compared to no recommendation. Conclusion: “The strong association between mask mandates and correct mask use suggests that public policy has a powerful influence on individual behaviour.”
In March 2022 when many mask mandates were being dropped an Angus-Reid/CBC poll found 73 per cent of Canadians would support continuing masking requirements in indoor public spaces. As I showed in Part 1, once authorities dropped the mandates, mask adherence plummeted.
A CTV/Nanos poll in November 2022 found 7 in 10 Canadians would support or somewhat support the return of mandatory mask wearing in public indoor spaces if authorities deemed it necessary.
3. Findings
There is widespread epidemiological evidence and study from the physical sciences that masks and mask mandates are associated with reductions in the transmission of SARS-COV-2 in a variety of settings.
There is further evidence that mask mandates are associated with reduced covid-19 hospitalizations and mortality.
There is evidence that higher population mask adherence and mask quality (eg N95) are associated with more effective reductions in transmission.
There is evidence that masking reduces respiratory virus transmission. However in-household masking recommendations* were found to be ineffective due to low mask adherence. (*This is the current advice of the CMOH of Ontario.)
There is little or no objective evidence that masks cause harms to children. Some areas like social and language development have mixed expert opinions and limited evidence.
There is evidence that the public is willing to return to mask mandates in indoor public spaces if authorities consider it necessary.
There is evidence that early this winter season Canada is sustaining an elevated level of Omicron infections, hospitalizations and deaths, a significant number of reported long covid health symptoms, extraordinary surges in respiratory illnesses among children, and extraordinary hospital issues (mostly due to pediatric RVI at present).
4. Discussion
Counter arguments to mask mandates
One argument is that ventilation, filtration, or vaccination can replace the need for masking.
Answer: The co-creator of the corsi-rosenthal box filter, Dr. Richard Corsi, has explained why masks are still needed to reduce risk. Aerosol scientists encouraging ventilation have done the same. Flu vaccines are < 60% protective vs infection, a first covid booster is < 60% protective vs symptomatic infection after 3 months. Meaning that those uncaught infections will spread to others, some more vulnerable. More practically, Canada continues to go through an elevated mass infection period at the current level of ventilation, filtration, and vaccination and change will not happen overnight.
A second argument is that Omicron’s high transmissibility weakens the ability of masks to prevent spread if indoor spaces can be saturated with infectious particles.
Answer: The high observed infection levels are with low, almost solo masking. The mask mandate evidence and physical science simulations highlight how high mask adherence and higher mask effectiveness can lower the reproduction number. That is why my mask article recommends N95 masks and a petition recommends the free distribution of those masks, just like rapid tests. The other key point is that current levels of immunity driven mostly by more recent infections and boosters have yielded relatively sustained levels of infections without public health precautions and messaging. That means the effective reproduction number cannot be too far above 1. Research evidence shows that mandates can lower R and that would lower or at least further slow the rate of infections.
A third argument is that much of the evidence on mask mandates is pre-Omicron and lacks strong randomized controlled trial (RCT) evidence.
Answer: In the real world involving complex human behaviour and pandemic decision timelines, waiting for a stream of perfect RCT studies is not feasible. Perfect is the enemy of good. I say that as a statistician. Masks are not a clinical trial drug. Still, the pre-Omicron scientific consensus supporting mandates is high and studies like the one out of Boston provide a glimpse of how mandates have the potential to reduce spread during Omicron as well, and that study depended on classic masking, not upgraded masking. We also need to consider that vaccines provide less protection against infection now and that masks are not only a defence against Omicron but a defence against respiratory disease surges.A fourth argument is that the harms are too great to reinvoke mandates.
Answer: I believe I have answered that argument in this article, in the section on children, argument #6 below, in the survey results on mask mandates, in my article on masks, and my point that mandates can be temporary and targeted.A fifth argument is that people are tired of masking and will not comply with a mask mandate, instead we should simply encourage them to wear masks.
Answer: I believe I addressed that in the section on public attitudes and behaviour as well as the description of what happened when people were encouraged to wear masks voluntarily (hint: masking dropped from 70% to 10%).A sixth argument is that there are children and adults who cannot wear a mask and should not be forced to wear one.
Answer: There should be flexibility and exceptions can be made.There is the argument that those who need to protect themselves from infection can wear a mask and others can decide for themselves.
Answer: I think I have explained how the science shows how important source control (someone infectious wearing a mask to contain their spread) is in limiting spread and how approximately half of the population may not know when they are infectious. Also, exposure to aerosols builds up over time and no mask is 100% protective.
Some argue that Canada should not be implementing something that the rest of the world is not doing.
Answer: I have three points: This article is based on Canadian data and science related to covid and mandates, not political science or copying some other place. Secondly, I have seen no jurisdiction provide objective reasons why a) they dropped mandates and b) why they have not returned to them when infection rates are high. Thirdly, I am seeing more and more jurisdictions and institutions beginning to return to mask requirements, including in the US and Canada.
Discussion
I believe the evidence is clear that the use of temporary and targeted mask mandates remains a safe and effective option to lessen the incidence of viral illness, hospitalizations and fatalities in Canada this winter. I also am encouraged by suggestive survey evidence that Canada is at a point where mask mandates could kickstart a rebound in masking in the highest risk indoor settings.
The population has many different segments, some with recent infections, some with recent boosters, some with low or high hospitalization risk, some with higher workplace or school risks, but the most important to protect are the “bookends” - the youngest and the oldest.
Our youngest are in urgent need of help as respiratory viruses surge past seasonal norms and young children overrun emergency departments and ICUs, some needing resuscitation, some even dying. Our seniors (and also other vulnerable people of all ages) are still dying in large numbers due to covid, numbers that have exceeded past years.
The group in the middle of the bookends may be least affected as far as hospitals but they are the parents of these children and the sons and daughters of these seniors. I believe they will pitch in when they understand that slowing transmission in public spaces will help those who most need to be protected and help to protect our health care system this winter. They may also not be fully aware of long covid risks and may face long covid consequences as they get repeatedly infected. This should be communicated to them by public health.
If authorities passively reintroduce mask mandates in a minimal number of settings for a token amount of pre-defined time with a set expiry date, we are likely to fail or achieve mediocre results. The Ontario CMOH’s example recommending parents mask in their homes to protect children is one such example, as I covered earlier in the evidence. As the Science Table brief on schools stated, isolated mandates only in schools would be problematic. Targeted indoor masking requirements would need to be in place to also limit community spread around schools and within households.
The onus is on authorities to be clear, decisive, and to lead in communications on mask requirements, vaccinations, and other measures to reduce spread like ventilation. They must be role models and not the opposite. The holidays are almost here and I anticipate a significant boost in infections over the holidays if nothing more is done. Indoor transmission is also higher in winter than other seasons.
I am not going to list all the high risk indoor spaces that would benefit from mask requirements but I will highlight some that I believe are good candidates given pre-Omicron data and studies, the three C’s of Crowded places, Closed spaces, and Close-contact settings, and areas with greater vulnerable populations: schools, universities, public transit, congregate living, health-related settings like doctor’s offices, pharmacies, grocery stores, concerts and other mass indoor event areas, indoor weddings and funerals, and stores subject to crowding during holiday shopping season. It would be good if employers recommended workplace masking during this time as well.
For mask mandates to work, there needs to be strong and committed leadership from the top to ensure there is timely action and targeting, clear goals, transparent sharing of science and evidence, helpful public education, widespread and active messaging, and ongoing communication. For mask mandates to be most effective the public should be educated on quality masks such as N95’s and they should be freely distributed and widely available. I started a petition on that.
These elements have been lacking in Canadian provinces in 2022, a year that has seen “manage your own risk” messaging at odds with the reality of record highs in Omicron infections, hospitalizations, and deaths, plus respiratory virus surges, all with little or no public health response outside of vaccination encouragement.
The steps shown in this graphic are key to the success and effectiveness of a mask mandate campaign and can potentially shorten the time a temporary mandate needs to be in place. If all these arrows go from empty triangles and boxes to empty circles and boxes, disinformation will increase, uptake will be minimized, and effective mask wearing will be diluted.
I hope this article has helped provide members of the public with the science and rationale behind the case for temporary and targeted mask mandates and why they can be an important tool to help deal with Canada’s current situation.
No one step will solve everything, but as Yogi Berra might say, doing nothing accomplishes nothing.
Bill Comeau is a retired and independent Canadian statistician with no ties to any organization, institution, company, or government. He has tracked covid-19 since the beginning of the pandemic. All work is public domain. He can be found at @billius27 on twitter and @billius27@mstdn.ca on Mastodon. Interactive Tableau data visualizations can be found at public.tableau.com/app/profile/bill.comeau.
Appendix - Mask Mandate Studies and Reviews
1. “Trends in County-Level COVID-19 Incidence in Counties With and Without a Mask Mandate — Kansas”, Nov 2020
“Countywide mask mandates appear to have contributed to the mitigation of COVID-19 transmission in mandated counties.”
2. “An evidence review of face masks against COVID-19”, Jan 2021
“we recommend increasing focus on a previously overlooked aspect of mask usage: mask wearing by infectious people (“source control”) with benefits at the population level, rather than only mask wearing by susceptible people, such as health care workers, with focus on individual outcomes. We recommend that public officials and governments strongly encourage the use of widespread face masks in public, including the use of appropriate regulation.”
3. “Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2”, Feb 2021
“At a hair salon in which all staff and clients were required to wear a mask under local ordinance and company policy, 2 symptomatic, infected stylists attended to 139 clients and no infections were observed in the 67 clients who were reached for interviewing and testing. During a COVID-19 outbreak on the USS Theodore Roosevelt, persons who wore masks experienced a 70% lower risk of testing positive for SARS-CoV-2 infection.4 Similar reductions have been reported in case contact investigations when contacts were masked5 and in household clusters in which household members were masked.6"
“Encouragement to follow social distancing measures for coronavirus disease 2019, plus either no mask recommendation or a recommendation to wear a mask when outside the home among other persons together with a supply of 50 surgical masks and instructions for proper use.”
”The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. The data were compatible with lesser degrees of self-protection.”
“Limitation: Inconclusive results, missing data, variable adherence, patient-reported findings on home tests, no blinding, and no assessment of whether masks could decrease disease transmission from mask wearers to others."
5. “The introduction of a mandatory mask policy was associated with significantly reduced COVID-19 cases in a major metropolitan city”, Jul 2021
“The mandatory mask use policy substantially increased public use of masks and was associated with a significant decline in new COVID-19 cases after introduction of the policy. This study strongly supports the use of masks for controlling epidemics in the broader community.”
6. “Strategies to minimize SARS-CoV-2 transmission in classroom settings: combined impacts of ventilation and mask effective filtration efficiency”, Jul 2021
“Infection probability estimates indicate that ventilation alone is not able to achieve probabilities <0.01 (1%). The use of moderate to high EFE masks reduces infection probability, >5× in some cases. Reductions provided by ventilation and masks are synergistic and multiplicative.”
7. “Safe traveling in public transport amid COVID-19”, Oct 2021
“Mandatory wearing of masks and practicing social distancing with masks during peak hours reduced infection rates by 93.5 and 98.1%, respectively.”
8. “Pediatric COVID-19 Cases in Counties With and Without School Mask Requirements - United States, July 1-September 4, 2021”, CDC MMWR Oct 2021
“The results of this analysis indicate that increases in pediatric COVID-19 case rates during the start of the 2021–22 school year were smaller in U.S. counties with school mask requirements than in those without school mask requirements.”
“Overall pooled analysis showed a 53% reduction in covid-19 incidence (0.47, 0.29 to 0.75), although heterogeneity between studies was substantial (I2=84%)”
10. “Modeling COVID-19 Mortality Across 44 Countries: Face Covering May Reduce Deaths”, Nov 2021
“This study's significant results show that face mask mandates were associated with lower COVID-19 deaths rates than the rates in countries without mandates.”
11. “Impact of community masking on COVID-19: A cluster-randomized trial in Bangladesh”, Dec 2021
“We found that mask distribution, role modeling, and promotion in a low- and middle-income country setting increased mask-wearing and physical distancing, leading to lower illness, particularly in older adults. We find especially robust evidence that surgical masks prevent COVID-19.”
12. “The Effectiveness Of Government Masking Mandates On COVID-19 County-Level Case Incidence Across The United States, 2020”, Feb 2022
“On average, the daily case incidence per 100,000 people in masked counties compared with unmasked counties declined by 25 percent at four weeks, 35 percent at six weeks, and 18 percent across six weeks post intervention. The beneficial effect varied across regions of different population densities and political leanings. The most concentrated effects of masking mandates were seen in urban counties; the benefit of the mandates was potentially stronger within Republican-leaning counties. Although benefits were not equally distributed in all regions, masking mandates conferred benefit in reducing community case incidence during an early period of the COVID-19 pandemic.”
13. “Association between Mask Mandates and Population-level COVID-19 Outcomes – What We Know So Far”, Mar 2022 (Public Health Ontario review of published research)
“The implementation of mask mandates has been associated with statistically significant reductions in COVID-19 case growth, hospitalizations and deaths. The information on adherence to mask mandates is limited and requires further study, but available evidence suggests that mask-wearing adherence increases when mask mandates are in place and that this adherence is associated with observed reductions in case growth.
Many of the studies that examined COVID-19 incidence, hospitalizations and deaths during periods in which mask mandates were implemented had layered infection prevention and control measures in place, so it is challenging to measure the independent impact of mask mandates. All studies included in this rapid review were performed prior to the emergence of the Omicron VOC and the availability and uptake of COVID-19 vaccination; thus, it is unclear whether certain findings are applicable to the current context.”
14. “SARS-CoV-2 Incidence in K-12 School Districts with Mask-Required Versus Mask-Optional Policies - Arkansas, August-October 2021”, Mar 2022
“Among districts that switched from no mask requirement to any mask requirement (full or partial), incidence among students and staff members decreased by 479.7 per 100,000 (p<0.01) upon implementation of the mask policy. In areas with high COVID-19 community levels, masks are an important part of a multicomponent prevention strategy in K-12 settings.”
15. “COVID-19 transmission in Hong Kong despite universal masking”, Apr 2022 “We conclude that universal mask-wearing can reduce transmission, but transmission can continue to occur in settings where face masks are not usually worn.”
16. “Relation of masking policy to COVID-19 positivity rate in Texas school districts”, Apr 2022
“Understanding of the impact of masking in schools to prevent COVID transmission is limited since much of the data considers factors in addition to masking. We collected data from 30 school districts in Texas, contrasting districts where masks were mandated with those where masks were optional. Results showed that mandatory masking was associated with a reduction in COVID-19 positivity among student populations, but not in staff populations.
17. “SARS-CoV-2 aerosol transmission in schools: the effectiveness of different interventions”, May 2022
“In the absence of interventions, the cumulative dose absorbed was 1.5 times higher in winter than in spring/summer, increasing chances of indoor airborne transmission in winter. However, natural ventilation was more effective in winter, leading to up to a 20-fold decrease in cumulative dose when six windows were fully open at all times. In winter, partly opening two windows all day or fully opening six windows at the end of each class was effective as well (2.7- to 3-fold decrease). In summer, good ventilation levels could be achieved through the opening of windows all day long (2- to 7-fold decrease depending on the number of windows open). Opening windows only during yard and lunch breaks had minimal effect (≤1.5-fold decrease). One HEPA filter was as effective as two windows partly open all day in winter (3-fold decrease) whereas two filters were more effective (5-fold decrease). Surgical face masks were very effective independently of the season (8-fold decrease). Combined interventions (i.e., natural ventilation, masks, and HEPA filtration) were the most effective (≥25-fold decrease) and remained highly effective in the presence of a super-spreader.
Natural ventilation, face masks, and HEPA filtration are effective interventions to reduce SARS-CoV-2 aerosol transmission. These measures should be combined and complemented by additional interventions (e.g., physical distancing, hygiene, testing, contact tracing and vaccination) to maximise benefit.”
18. “Mask wearing in community settings reduces SARS-CoV-2 transmission”, May 2022
“We find that mask wearing is associated with a notable reduction in transmission. Our evidence shows that factors other than mandates must have contributed to the worldwide uptake of mask wearing in 2020. In situations where mandates are unlikely to have a large effect on uptake—for example, because voluntary wearing is already high—policy makers may be able to use other levers to increase wearing quantity and quality. For example, if masks are widely used but are often of poor quality, or worn incorrectly, or are not worn in the most important venues, then policy makers can respond with education about correct mask fitting and quality, as well as mandates that focus on venues with the greatest risk of transmission.
19. “School Masking Policies and Secondary SARS-CoV-2 Transmission”, May 2022
”A total of 1 112 899 students and 157 069 staff attended 61 K–12 districts across 9 states that met inclusion criteria. The districts reported 40 601 primary and 3085 secondary infections. Six districts had optional masking policies, 9 had partial masking policies, and 46 had universal masking. In unadjusted analysis, districts that optionally masked throughout the study period had 3.6 times the rate of secondary transmission as universally masked districts; and for every 100 community-acquired cases, universally masked districts had 7.3 predicted secondary infections, whereas optionally masked districts had 26.4.”
20. "Impact of local mask mandates upon COVID-19 case rates in Oklahoma", Jun 2022
“Compared to rates in communities without mask mandates, transmission rates of SARS-CoV-2 slowed notably in those communities that adopted a mask mandate.”
21. “District-Level Universal Masking Policies and COVID-19 Incidence During the First 8 Weeks of School in Texas”, Jun 2022
“Texas discontinued state-sponsored business restrictions and mask mandates on March 10, 2021, and mandated that no government officials, including public school officials, may implement mask requirements even in areas where COVID-19 hospitalizations comprised more than 15% of hospitalizations. Nonetheless, some public school districts began the 2021-2022 school year with mask mandates in place. We used quasi-experimental methods to analyze the impact of school mask mandates, which appear to have resulted in approximately 40 fewer student cases per week in the first eight weeks of school.”
22. “Lifting Statewide Mask Mandates and COVID-19 Cases: A Synthetic Control Study”, Jul 2022
“Lifting the mask mandate in Iowa was associated with an increase in new COVID-19 cases. Caution should be applied when making this type of policy decision before having achieved a more stable control of the pandemic.”
“These results suggest that in-class transmission of SAR-CoV-2 in an urban university with masking and vaccine protocols in-place was negligible.”
24. “Unravelling the role of the mandatory use of face covering masks for the control of SARS-CoV-2 in schools: a quasi-experimental study nested in a population-based cohort in Catalonia (Spain)”, Aug 2022
“We found no significant differences in SARS-CoV-2 transmission due to FCM mandates in Catalonian schools. Instead, age was the most important factor in explaining the transmission risk for children attending school.”
25. “Mask-wearing in Children and COVID-19… What We Know So Far”,
Aug 2022 (Public Health Ontario review of published research)
- “Studies have shown that schools with masking policies have been associated with lower incidence of severe acute respiratory coronavirus 2 (SARS-CoV-2) infection compared to schools without mask mandates for children. - “Studies evaluating child adherence to masking policies have shown similar results in school (range from individual studies: 43%–97%) and community settings (34%–96%), with increased adherence as age increased.”
- “There was no objective evidence for reduced respiratory function in children who wore masks, with commonly reported complaints being subjective. There was no evidence of negative cognitive impacts and there were mixed results for studies on the psychological, communicative and dermatologic impacts of child mask-wearing.”
26. “Infection Prevention and Control Considerations for Schools during the 2022-2023 Academic Year”, Aug 2022 (Ontario Science Table Brief)
“Temporary infection-related health and safety measures (e.g., masking, physical distancing, cohorting, active screening, testing) can help reduce the transmission of communicable illnesses in schools. However, some can pose additional challenges to school operations, student learning and student wellness. Furthermore, some of these measures may adversely impact social connectedness, which is of vital importance for children of all ages and of heightened significance in the adolescent years. Therefore, a thoughtful approach based on real-time local level analysis is recommended before reintroducing these temporary measures after careful consideration of the potential benefits and negative consequences. Given that schools are not isolated from communities, implementation of these temporary measures should not be done in isolation of community measures for indoor spaces. These temporary measures are not expected to be required at the start of the 2022 school year.”
27. “Risk of SARS-CoV-2 Acquisition in Health Care Workers According to Cumulative Patient Exposure and Preferred Mask Type”, Aug 2022
“Consequent use of respirators and SARS-CoV-2 vaccination might substantially decrease the work-related risk for HCWs exposed to patients with COVID-19.”
28. “Association of masking policies with mask adherence and distancing during the SARS-COV-2 pandemic”, Sep 2022
“Of 109,999 individuals observed in 126 US cities, 48% wore masks correctly with highest adherence among females, teens and seniors and lowest among non-Hispanic whites, those in vigorous physical activity, and in larger groups (P < .0001). Having a local mask mandate increased the odds of wearing a mask by nearly 3-fold (OR = 2.99, P = .0003) compared to no recommendation.”
“Rt decreased after mask mandate during the region's case-count spike suggested reduction in SARS-CoV-2 transmission.”
30. “The Association Between State-Issued Mask Mandates and County COVID-19 Hospitalization Rates”, Nov 2022
“This study demonstrated that state-issued mask mandates were associated with reduction in COVID-19 hospitalizations across the United States during the earlier portion of the pandemic. As new variants of the virus cause spikes in COVID-19 cases, reimposing mask mandates in indoor and congested public areas, as part of a layered approach to community mitigation, may reduce the spread of COVID-19 and lessen the burden on our health care system.”
31. “Lifting Universal Masking in Schools - Covid-19 Incidence among Students and Staff”, Nov 2022
“Among school districts in the greater Boston area, the lifting of masking requirements was associated with an additional 44.9 Covid-19 cases per 1000 students and staff during the 15 weeks after the statewide masking policy was rescinded. This estimate corresponded to an additional 11,901 Covid-19 cases (95% CI, 8651 to 15,151), which accounted for 33.4% of the cases (95% CI, 24.3 to 42.5) in school districts that lifted masking requirements and for 29.4% of the cases (95% CI, 21.4 to 37.5) in all school districts during that period.”
Respiratory Viruses:
32. “Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis”, May 2020
“This meta-analysis of the 21 studies provided the latest state-of-art evidence on the efficacy of masks in preventing the transmission of RVIs. Our data show that the protective effects of masks against RVIs were not only significant for both HCWs and non-HCWs, but also consistent between Asian and Western populations.”
33. “Face Mask Use and Control of Respiratory Virus Transmission in Households”, Feb 2009
“We found that adherence to mask use significantly reduced the risk for ILI-associated infection, but <50% of participants wore masks most of the time. We concluded that household use of face masks is associated with low adherence and is ineffective for controlling seasonal respiratory disease.”
















You are a beacon of light for all people searching for guidance. My family relies on you to obtain truth and clarity in learning how to navigate in these murky Covid waters. No person could ever thank you enough for all your generous work. God bless you!
Thank you Bill. Will be sharing the link to this. Your work is much appreciated.