The science behind masks and their use
Evidence for masks, why they work, which work best, how to use them, and when and where they are most needed.
Background
In early September I and others warned about the upcoming Fall and Winter seasons and the potential for heightened infection risks particularly in indoor public spaces. This article draws from a twitter thread I wrote on September 13, 2022. It is intended to share evidence, advice, and reminders on how to up your game when it comes to masks and the handling of elevated airborne risks.
Covid is Airborne
Let's start by going back to a basic principle: Covid is airborne, something WHO has been slow to communicate or acknowledge.
we were not forcefully saying: “This is an airborne virus.” I regret that we didn't do this much, much earlier - WHO’s chief scientist, 11/23/2022
Particles come in all sizes; definitions for droplets are arbitrary. The closer you are to an infected person, the more you are exposed to more viral-laden particles. But you can still be infected by a build up of aerosols at further distance in less ventilated areas.
The 6' and 15 minute contact rules are outdated and developed arbitrarily by WHO and the CDC et al in 2020 for the less transmissible Wuhan strain and based on droplets. Omicron can infect in much less time and distance depends on many factors, including the size of the aerosols, airflow, and ventilation. Experiments physically confirm that a mask worn at the source reduces the generation of aerosols, as one would expect. There is also currently little or no scientific evidence that surface fomites are a meaningful vector for Omicron transmission.
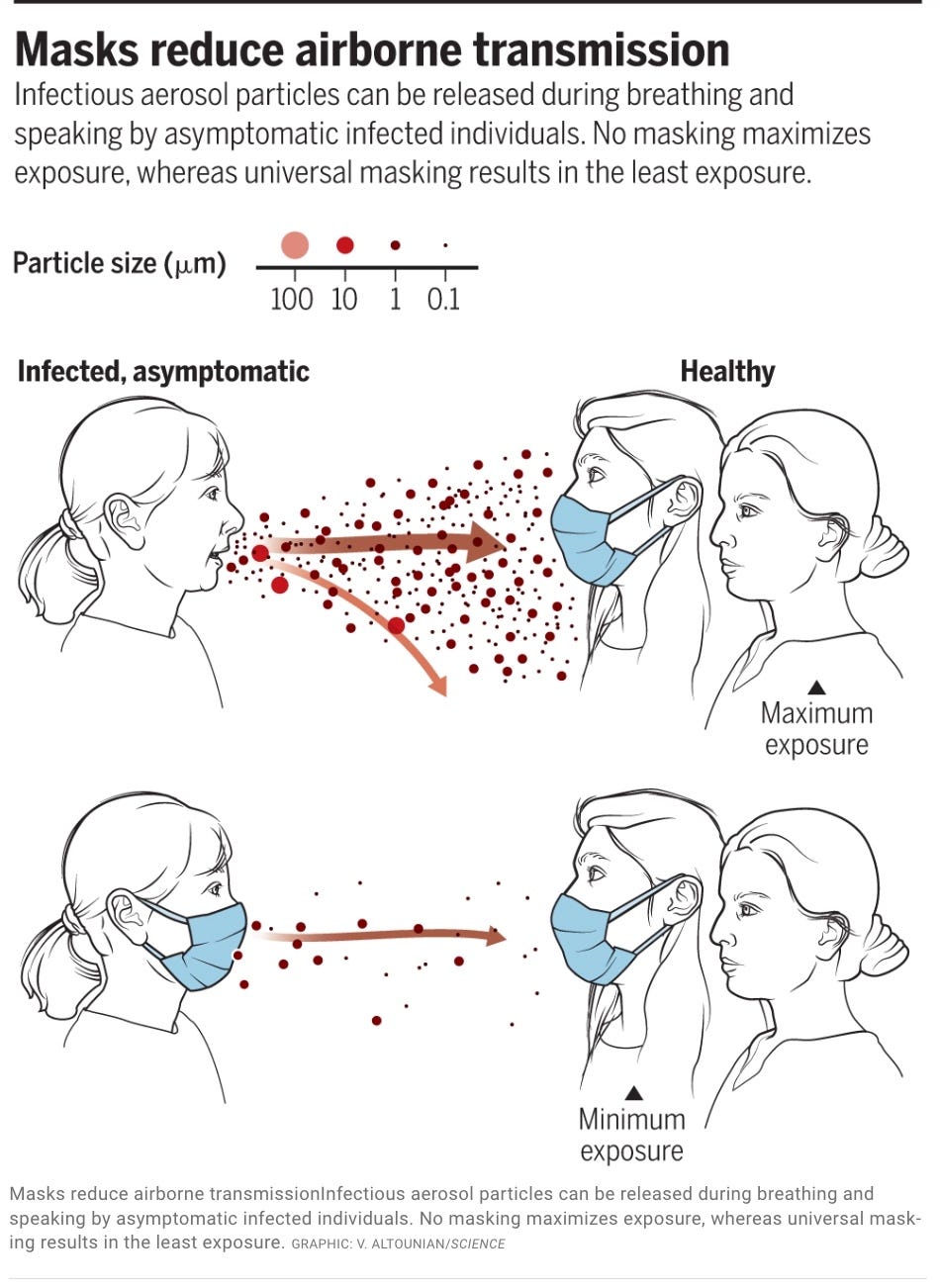
This graphic is from an important paper in Science, “Airborne transmission of respiratory viruses”.
Engineers and aerosol scientists like Dr. Kimberley Prather, a Distinguished Chair in Atmospheric Chemistry, have also reinforced the physical science and confirmed the benefits of masking, not just to help protect the wearer but to protect others, even when you may be asymptomatic and unaware you are infectious.
Mask Research
The broad consensus of peer-reviewed and published science has been straightforward: masks work. The degree depends on issues like real world compliance, study design, type of masks, and other factors.
Here is a list of 27 peer-reviewed and published mask studies. Of these, 22 studies find masks are effective, 1 is inconclusive, and 4 find masks generally ineffective. (It is important that we set standards on what studies to review, since there are libertarian and disinformation faux institutions attempting to cherry pick, or “publish” skewed reviews of mask studies and evidence.)
Those still debating whether masks work may claim that there are few if any Randomized Clinical Trial (RCT) studies. While there was a large RCT study in Bangladesh of villagers that found benefits with surgical masks, the more important point is this: you cannot force people in the real world to consistently wear masks or not wear masks in situation A, setting B, and infection risk level C. It would also be unethical to ask some people to not wear masks in a known contagious or higher risk setting. The closest we can really come is with controlled environment aerosol “mannequin” experiments and carefully analyzed real world comparisons. This article wryly mocks the RCT argument: “Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomized controlled trials.”
Masks range from low to high technology when it comes to protecting against airborne transmission.
Early in the pandemic, there was evidence on the superior performance of N95 masks, something the NY Times wrote about at the time. A study published in Applied Physical Sciences examined the Total Inward Leakage (TIL) of various respirator (FFP2) and surgical mask options. Surgical masks had predictably more leakage.
It is also very important that masks have good filtration ability against airborne viral particles. This study found N95 masks to be superior to surgical masks: "N95 masks with suboptimal fit still had comparable filtration efficiency of more than 90% … Surgical masks secured with either ties or ear loops also had much lower filtration efficiency of 37% to 69%."
The more your mask leaks or fails to filter airborne particles, the less effective it is against Omicron and respiratory virus transmission. This is why a recently published Swiss study found respirators such as N95 masks to be superior to surgical masks for health care workers. [Throughout this blog, the term “N95” may be used interchangeably with “FFP2”, “respirators” and include variations like KN95, KN94, and CAN95.']
This is reinforced by a CDC-cited California study that found people who wore N95/KN95 masks had a much lower risk of infection. While those wearing any form of mask had lower infection rates than maskless, there was a clear improvement when people wore surgical masks and a further improvement when they wore N95/KN95 masks.
Why do N95 masks work when viral particles are so small? One of the biggest hurdles in public acceptance is getting past disinformation and myths that quality masks do not work, eg viral particles are too small. In fact, the viral particles do not travel solo, they hitchhike on mucosal or other larger airborne particles. N95 mask filters include multilayered technology that both attracts particles while also exploiting the physics of their brownian motion. This three minute video can help family and friends understand why the science and technology behind an N95-level mask does in fact work.
One of the top US experts on masks, Jeremy Howard, has written extensively about the benefits of masking. He includes advice on masks and their use that I will touch on in the next section.
“I led the team that studied mask efficacy in early 2020 and published our results in the Proceedings of the National Academy of Science. I spent three months earlier this year revisiting this topic, and today I'm publishing my notes and links here” - Jeremy Howard
Wearing masks
Since our goal is to minimize the inhalation of infectious aerosols, the fit and effectiveness of a mask seal to the face is important.
Factors that can improve that seal include your choice of mask quality, proper size, comfort, having straps that go around the head (not ear loops), being clean-shaven, and knowing how to do a basic user fit as shown in this demonstration:
The evidence we have suggests that the greater the quality of masks against airborne transmission, the greater the reduction in transmission risk. Two factors drive mask performance: filtration and fit.
Though better than going maskless, cloth masks are less effective since they are least likely to fit well and offer the least filtering. Surgical masks are better than cloth and are designed to protect against fluid droplets and spray. They are best suited for close medical settings. However, blue surgical masks are loose at the sides and not designed to fit the face although there are a couple ways to improve their fit, as Jeremy Howard listed:
Knot and Tuck: Tying the sides of the mask together to remove the side gap
Double masking: Wearing a tight fitting cloth mask over a surgical mask”
N95 masks, on the other hand, are designed to provide a high level of aerosol filtration and are designed to fit the face. (I encourage squeezing at the nose bridge to reduce air gaps, using head straps as opposed to versions with ear loops, and checking the basic user fit video I provided earlier.)
Jeremy Howard encapsulated an ACGIH summary on relative mask performance:
“N95 filtering face piece respirator… has 1-10% inward leakage and outward leakage”, but with a surgical mask “has 50% inward leakage and outward leakage”, and with a cloth face covering “has 75% inward leakage and outward leakage”.
Reusing N95 masks
Many people are unclear on how long they can wear N95 masks or reuse them. 3M explains: ”There is no time limit to wearing an FFR. Respirators can be worn until they are dirty, damaged or difficult to breathe through.”
Peter Tsai, the inventor of N95 masks, came out of retirement to provide advice on how to reuse them:
- Use 3–4 masks, numbered on the outside as 1–4, for each day. They can be used each day in numerical order. All SARS-CoV-2 viruses on the mask will be dead in 3 days. Masks should be kept at room temperature (21–23°C [70–73°F]) and 40% humidity. There is no change in the mask's properties.
- N95 Masks Can be Heated at 70°C (158°F) for 60 Min
- NOT RECOMMENDED: Using Soap and Water (54% FE) and Alcohol (67% FE)
Masks for children
From the CDC:
”Masks and respirators should not be worn by children younger than 2 years. Choose a high-quality and comfortable mask or respirator that your child can wear properly. A poorly fitting or uncomfortable mask or respirator might be worn incorrectly or removed often, and that would reduce its intended benefits. Choose a size that fits over the child’s nose and under the chin but does not impair vision.”
The American Academy of Pediatrics supports masking for children 2 and older and answers common questions parents have here: HealthyChildren.org.
Public Health Ontario reviewed mask use in children and concluded “schools with masking policies have been associated with lower incidence of severe acute respiratory coronavirus 2 (SARS-CoV-2) infection compared to schools without mask mandates for children” and also “there was no objective evidence for reduced respiratory function in children who wore masks, with commonly reported complaints being subjective. There was no evidence of negative cognitive impacts and there were mixed results for studies on the psychological, communicative and dermatologic impacts of child mask-wearing.”
The New York Times published an article on child learning while masked:
”Even parents who support mask mandates often worry about how a school year without smiles and frowns might negatively affect their children. These concerns are understandable but unwarranted. Although scientists don’t have much data yet on how wearing masks during a pandemic affects children’s development, there is plenty of reason to believe that it won’t cause any harm.” Dr. J. Danovitch, research psychologist who studies the cognitive and social development of children. NY Times 8/18/21
There are several N95-level products designed for children. Adult masks or cloth masks are not recommended except as a less effective option. The important thing is that they are comfortable for the child and the child knows how to wear them properly.
N95 costs
N95 masks are less understood by the general public and do cost more and for those reasons I will list two initiatives (although it is important to recognize that N95’s are reusable which brings the usage cost down considerably).
- I started a petition in October to have N95 masks distributed to Canadians free-of-charge in preparation for the winter covid and respiratory season. Over 10,000 Canadians have signed. You are welcome to add your signature and contact your MP or the Minister of Health of Canada, Jean-Yves Duclos.
- Donate a Mask accepts donations and can provide quality masks to those in need
Assessing Indoor and Outdoor Risks
You should consider wearing a mask when infection levels are elevated and hospitals are under stress or when you are at higher risk of infections in your daily activities or work, or if you have a higher risk of severe health outcomes from infection.
There is a myth that vaccines are 100% protective against Omicron or respiratory virus infections, so masks are unnecessary. This is untrue. Vaccines can lower risk but there is plenty of room left to get infected, especially with Omicron variants which cause vaccine doses to wane over time. Masks are simply a way to boost your protection and complement the less-than-perfect risk reductions that vaccines deliver. I recommended that the public relies on independent data and science to help assess their risk, and not just the opinions of government officials, employers, or members of the public.
Different public settings carry different risks depending on whether you are indoors or outdoors, the level of ventilation, how crowded or busy the location is, the length of time exposed, and the level of activity. (Room filtration like HEPA filters are not shown here but would reduce risk.) All risks, including exposure time, are also heightened with Omicron. This same table can also apply to any respiratory virus, such as flu or RSV although Flu and RSV infection risk can also be reduced by cleaning surfaces and good hand hygiene. Omicron, however, shows no evidence that surface fomites are a vector for transmission. That’s why masks are the top personal protection layer after vaccination.
Where might it be more critical to mask? It partly depends on the level of ventilation and filtration at a location. But on average there are certain types of public indoor locations and settings that are more likely to present a higher risk based on studies, contact tracing, the greater presence of sick or vulnerable people, and the “3 C’s” (crowded places, closed spaces, close contact). These include: health care settings, congregate living and retirement homes, pharmacies, mass transit, taxis, schools, concerts and movies, certain workplace environments, social gatherings like weddings, funerals, and holiday parties, mass indoor events, and more crowded store environments. (Gyms, bars, and restaurants have been ranked as high risk but it’s difficult to mask in those settings.)
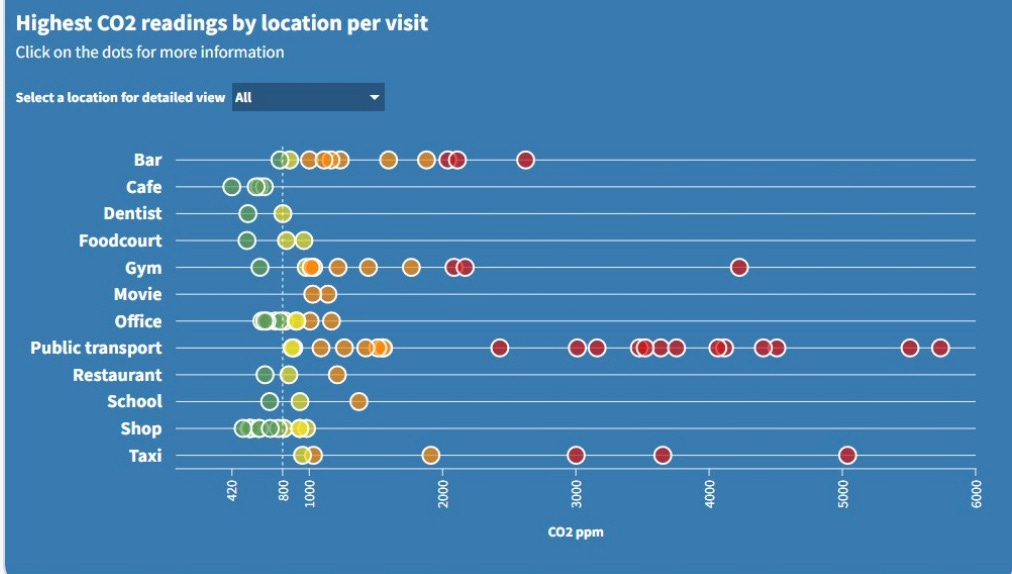
Masking is more important when an indoor location has poor or unknown ventilation. One way to measure that risk is a portable CO2 monitor. It lets you know how much indoor air is being rebreathed due to a lack of ventilation. If someone is infectious in a room, your inhalation of viral particles will be greater when the CO2 reading is higher.
This chart shows a volunteer’s sampling of CO2 readings in different settings. Tools like the Raven App can also provide clean air maps based on CO2 readings.
I am sometimes asked about the need for outdoor masking. The one (pre-Omicron) study I have read in the Journal of Infectious Diseases suggests that indoors represents an 18.7 times higher risk than outdoors (95% confidence interval, 6.0–57.9). But that depends on the nature of the indoor or outdoor activity. The study summarizes: “These results suggest that moving activities to outdoor settings may reduce infections and ultimately save lives. However, it is important to note that infections are possible outdoors and the advantage may be overtaken by relaxed mitigation efforts.”
I see some, including some school administrators wondering if HEPA filters mean masks are not needed (eg schools). Creators of the #corsirosenthalbox and aerosol scientists strongly recommend masking as an additional layer of protection. This is especially true with the more transmissible and evasive Omicron variants.

Two-way risk
The Max Planck fluid dynamics study, the CIDRAP report, and studies showing a high percentage of people are not always aware they are infectious, all combine to point to increased risk for others if you are unmasked, whether they are masked or not.
The table below is based on CIDRAP and other sources. You can see from this that N95 masks, even when not fully fitted, perform better than surgical masks (SM) and cloth. You can also see that it’s critical that someone who is infected (even if they are unaware) wears a mask to reduce the risk to someone who is not infected, even if they are wearing a mask. With Omicron, the time to reach an infectious dose is much less, so the quality of mask is even more important. No mask will reduce your risk to zero against Omicron, it depends on the risk situation you are in and the length of time you are exposed to viral particles.
Are there alternatives to masking? There are, they are just not very attractive options in the short-term. We could ensure all high risk indoor public spaces meet ventilation, filtration, or Far UV engineering standards and display CO2 readings but that would take time and money. We could close businesses, transit, and schools that are high risk, causing significant harm to them and the public. We could depend solely on vaccines but the current variants and respiratory viruses like flu partly evade vaccines so many are still getting infected and not all viruses have vaccines, like RSV.
Beyond N95 masks
The cleanaircrew.org website is a good resource for masks. I currently wear a 3M N95 Aura but there are several other N95-level options (like KN94/95, CAN95, etc).
Beyond N95’s there are even higher protection FFP3/N99 and elastomeric masks that increase filtration and fit performance even further. They may also include the option of replacing the filter.
Cambridge University’s hospital research on FFP3’s:
“Once FFP3 respirators were introduced, the number of cases attributed to exposure on COVID-19 wards dropped dramatically – in fact, our model suggests that FFP3 respirators may have cut ward-based infection to zero.”
Summing up
The decision to wear a mask is a personal decision in most settings now and that may depend on a community’s level of infections, the risk in a particular setting, the status of hospital care, and each individual’s personal assessment of their risk and those around them.
What this blog has attempted to do is to help make that mask decision as informed as possible by recounting published and peer-reviewed scientific evidence, debunking some myths, and sharing advice on personal mask selection and use, in particular, the recommendation to choose well-fitting N95-level quality masks when it comes time to wearing a mask in public spaces.
Just like vaccines, masks don’t completely prevent infection from Omicron or respiratory viruses but if properly used, they can reduce the risk for you and those around you.
Bill Comeau is a retired, independent, Canadian statistician with no ties to any organization, institution, company, or government. He has tracked covid-19 since the beginning of the pandemic. All work is public domain. He can be found at @billius27 on twitter and @billius27@mstdn.ca on Mastodon.
















Brilliant article! I hope it reaches as many people as possible to educate on why masks work! Thank you for doing this!👏👏🤗🤗
Thanks Bill, clear and concise, hope lots of people take the time to read and make a proper evaluation of not just their personal circumstances but also of those they come in contact with.